Thoracic Outlet Syndrome (TOS)
- Home
- Arm
- Common Ailments
- Thoracic Outlet Syndrome (TOS)
Thoracic Outlet Syndrome (TOS) is defined as a group of signs and symptoms that collectively characterize or indicate a particular disease or abnormal condition involving the neck, shoulder and arm.
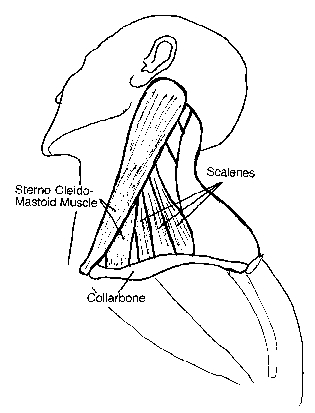
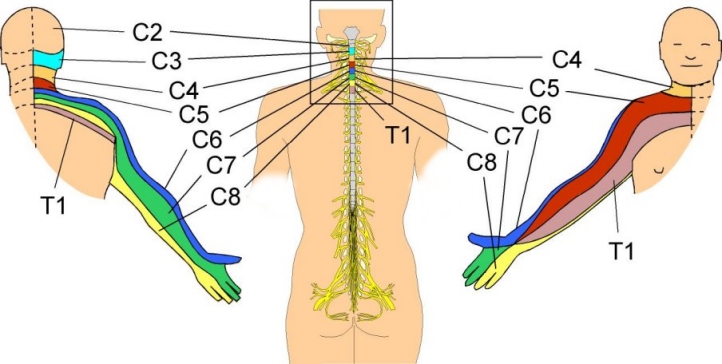
This diagram shows the anatomy involved with TOS. The main anatomy features are those that collectively makeup the NEUROVASCULAR BUNDLE; these consist of brachial plexus (plus the C8 and T1 nerve roots) and the subclavian artery and vein.
- The brachial plexus (coloured yellow) is the network of motor and sensory nerves which innervate the arm, the hand, and the region of the shoulder girdle.
- The vascular component of the bundle, the subclavian artery (coloured red) and vein (coloured blue) transport blood to and from the arm, the hand, the shoulder girdle and the regions of the neck and head.
Compression occurs when the size and shape of the thoracic outlet is altered. The outlet can be altered by exercise, trauma, pregnancy, a congenital anomaly, an exostosis, postural weakness or changes.
Below is a list of the component syndromes which comprise thoracic outlet syndrome along with a brief description of each.
- Anterior scalene tightness – compression of the interscalene space between the anterior and middle scalene muscles-probably from nerve root irritation, spondylosis or facet joint inflammation leading to muscle spasm.
- Costoclavicular approximation – compression in the space between the clavicle, the first rib and the muscular and ligamentous structures in the area-probably from postural deficiencies or carrying heavy objects.
- Pectoralis minor tightness – compression beneath the tendon of the pectoralis minor under the coracoid process-may result from repetitive movements of the arms above the head (shoulder elevation and hyperabduction).
It is important to understand that presenting with the symptoms listed below in no way indicates a definitive diagnosis for thoracic outlet syndrome. Professionals understand the importance of coupling diagnostic testing skills with the patient’s report of what hurts and what doesn’t seem to be working properly. Don’t self diagnose! Neurologic and vascular symptoms can be indicative of more serious conditions.
- Vascular TOS (caused by compression of the subclavian artery or vein)
- Neurogenic TOS (caused by compression of the brachial plexus)
Vascular symptoms include:
- Swelling or puffiness in the arm or hand
- Bluish/white discoloration of the hand
- Feeling of heaviness in the arm or hand
- Pulsating lump above the clavicle
- Deep, boring toothache-like pain in the neck and shoulder region which seems to increase at night
- Easily fatigued arms and hands
- Superficial vein distention in the hand

Neurologic symptoms include:
- Parasthesia along the inside forearm and the palm (C8, T1 dermatome)
- Muscle weakness and atrophy of the gripping muscles (long finger flexors) and small muscles of the hand (thenar atrophy is known as Gilliatt-Sumner hand and intrinsics)
- Difficulty with fine motor tasks of the hand
- Cramps of the muscles on the inner forearm (long finger flexors)
- Pain in the arm and hand
- Tingling and numbness in the neck, shoulder region, arm and hand
Non-specific or disputed TOS (in which the pain comes from unexplained causes)
Non-specific TOS most prominently features a dull, aching pain in the neck, shoulder, and armpit that gets worse with activity. Non-specific TOS is frequently triggered by a traumatic event such as a car accident or a work related injury. It also occurs in athletes, including weight lifters, swimmers, tennis players, and baseball pitchers.
There is no definite treatment for TOS, however physiotherapy can provide the vital skills and education for management of the condition.
- Posture education – is essential for long term management to help increase the thoracic space where nerves and arteries can become compressed
- Specific exercise program – to stretch shortened muscles that may be compressing and strengthening weak muscles including the chest muscles and deep neck flexors
- Medication – maybe prescribed to help with the pain
- Surgery – as a last resort surgery can be offered to decompress the structures that have become compressed
