Plantar Fasciitis
- Home
- Foot
- Common Ailments
- Plantar Fasciitis
Plantar Faciitis is a common, inflammatory condition of the foot. It accounts for 80% of heel pain, with a lifetime prevalence of 10%. It is common in people 40-60 years of age, and twice as common in women as men.
The plantar fascia is a thick, ligamentous connective tissue that runs from the heel bone to the ball of the foot. This tissue is strong and tight and contributes to maintaining the arch of the foot. It is an important transmitter of the weight across the foot as you walk or run.
When a patient has plantar fasciitis, the connective tissue that forms the arch of the foot becomes inflamed (tendonitis) and degenerative (tendinosis) – together these abnormalities cause plantar fasciitis.

- Typically affects people 40-60 years of age
- Overweight or obese
- People who are on their feet for extended periods; walking or standing on hard surfaces
- Poor footwear; especially high heels or unsupportive flat shoes e.g. flipflops
- People who walk or run for exercise, especially if you have tight calf muscles that limit how far you can flex your ankles
- People with very flat feet or very high arches are also prone to plantar fasciitis

- Often patients report insidious onset of pain well localised over the heel area of the bottom of the foot
- Symptoms are typically worse early in the morning after sleep
- Symptoms will occur after prolonged periods of sitting, or when walking in non supportive shoes
- Patients will often complain of a tightness along the sole of their foot and in their calf.

- Rest the foot. Until the morning pain settles to an acceptable level you must avoid aggravating factors i.e. running, excessive walking and/or standing and undue stretching of the sole. Gentle walking in supportive shoes and calf stretches as described below are fine.
- Correct, supportive footwear are essential in the management of plantar fasciitis. Chose shoes that have support around the ankle and arch, and a cushioned heel. You may also find a slight heel more comfortable than flat shoes. Avoid flat ballet pump type shoes, slippers and sandals without support around the ankle or arch.
- Heel pads and orthotics help to cushion the heel and support the arch of your foot. These will work best when worn in your shoes at all times.
- Painkillers and anti-inflammatory medication can be useful if the foot is particularly painful. Anti-inflammatories are particularly useful in the acute phase of the condition.
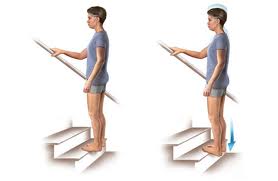
- Stretches to the achilles tendon and plantar fascia will help ease the symptoms in most people. People with plantar fasciitis often have a tightness of the achilles tendon; resulting in a knock-on effect of keeping the plantar fascia tight. During the night or when resting the plantar fascia tends to tighten up which is why it is usually most painful to stand first thing in the morning or after a period of rest.
- Night Splint can be worn to help keep the achilles tendon and plantar fascia ‘stretched’ so that these two structures are not put under tension when placing the foot on the floor first thing in the morning.
- Icing the sole of the foot by rolling a cooled bottle or tin will help ease the inflammatory symptoms.
Other treatment options include taping, ultrasound, injection and at a last resort surgery.
Physiotherapy treatment can be successful in the treatment of plantar fasciitis. Our aim as physiotherapists is to teach the patient management techniques to help them to control the symptoms. We offer hands on treatment in the form or soft tissue release, joint mobilisations if necessary, taping, ultrasound and importantly stretching and strengthening. We also pride ourselves in offering advice and education for the patient who wishes to return to their chosen sport.